Validating and Loading Elections
This section provides an overview of validation and loading and discusses how to:
Force-finalize participant events.
Find prepared participants who qualify for termination.
Find employees with late enrollment forms.
Post elections to Base Benefit tables.
When the Benefits Administration process validates and loads elections associated with participant events, it reevaluates the events in much the same way that it did during the option preparation phase. The difference is that the participants have had a chance to update their benefit election information and their choices have been entered into the system.
The system evaluates the updated benefits information using the same set of eligibility rules and event rules that it used to determine options. It also recalculates benefit election defaults where appropriate. This is important because these defaults may possibly have changed if events are processed out of sequence, or if changes are made to Base Benefit tables in the interim between runs of the Benefits Administration process. In this case, the recalculated defaults may not match the defaults shown on enrollment forms or inquiry pages.
During finalization, the system also assigns excess credits to plans in which the participant is enrolled. If the participant event processes correctly, it loads the new option elections and related information to the Base Benefits tables that store benefits information for the associated participant. It creates rows for new, changed, or terminated benefit option enrollments, but only if the new enrollment is different from the existing enrollment. (That is, simply reelecting an existing coverage does not generally cause a new row to be inserted into Base Benefit tables if all election-related data is the same).
Processing errors during validation and loading might be caused by:
Problems with the new election information that was entered into the system during data entry.
HR information linked to the participant event.
The design of the related eligibility rules, the event rules, or benefit program associated with the event.
You need to evaluate the error to determine whether anything needs to be fixed. If only the employee's election data needs to be corrected, then an event in EE status will be picked up for further processing during the next run of the schedule. However, if you need to correct the employee's HR data (which could affect his benefits eligibility), or if you need to correct the underlying benefits rules or setup, then the event must be specifically reprocessed back to the first phase of benefits processing (scheduling, event assignment, or option preparation).
Note: Event Maintenance and Open Enrollment schedules are processed the same way during validation and loading.
When you tell the system to finalize a participant event, it brings that event to an FE process status, even if it has been processed with errors. If the event is at a process status of ET or EE (election error), the system loads the participant's valid elections to the Manage Base Benefits business process tables. If the event is at any other process status, the system applies the appropriate default elections and loads them into the Base Benefit tables. The system also applies and loads default elections to replace elections that have been made in error.
You can force-finalize individual participants with the Final check box on either the Event Status Update page or the Controls page of the Processing Controls Update component. On the next run of the Benefits Administration process, the system automatically force-finalizes all participants with the Final check box selected.
If you're processing an Open Enrollment schedule, you can force-finalize all of the participants within that schedule. You'll arrange this when you set up the run control for the Benefits Administration process.
Open Enrollment schedules can be force-finalized because this method fits in with the nature of the Open Enrollment process, which has a finite set of start and end points. At the end of the enrollment period, you would force-finalize any employees who hadn't yet made their elections. Presumably, the open enrollment event rules that you create would enforce your business policies regarding failures to make positive elections (or reelections) in certain critical or regulated plan types.
Event Maintenance schedules, on the other hand, are processed on an ongoing basis. Each employee in a typical Event Maintenance schedule can be associated with a variety of different events and triggered actions at a given point in time. As you process certain events for the participant, more events are triggered for later Event Maintenance processing. The Event Maintenance procedure has no end, so enabling the forced finalization of an entire Event Maintenance schedule does not make sense isn't reasonable.
When the Event Maintenance process is run, participants can be identified as qualifying for termination when their participant events reach a process status of PR. The benefits administrator must terminate these employees manually by force-finalizing them.
The Find Terminations Workflow process locates participant events at a process status of PR that qualify for termination after Event Maintenance processing but who have not yet been manually terminated. It then makes a list of these participant events and sends it to the benefits administrator.
Set this workflow in action through the Process Scheduler by selecting
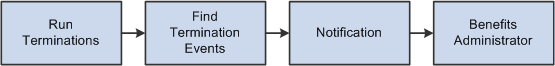
This chart illustrates the Find Terminations Workflow process:
This image describes the Find Terminations Workflow process.
When event maintenance is run, a set of notification letters and election forms are sent out to new employees and to employees whose coverage has changed due to a specific event. The Find Late Enrollments workflow retrieves a list of the employees who have not returned their benefits enrollment forms. Find Late Enrollments brings you to the Event Status Update page, where you can select the Final check box to assign default coverage for these employees.
Set this workflow in action through the Process Scheduler by selecting
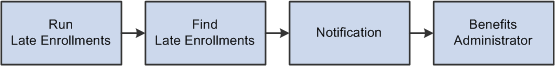
This chart illustrates the Find Late Enrollments Workflow process:
This image illustrates the Find Late Enrollments Workflow process.
For additional information, see the product documentation for: PeopleTools: Workflow Technology
As elections are prepared for posting to the Base Benefit tables, Benefits Administration determines the proper coverage begin dates and deduction begin dates based on event rules defined by plan type. Future-dated elections are inserted into Base Benefit tables as the participant elections are validated or finalized.
Payroll processes such as the Payroll for North America Pay Calculation process select elections based on effective date, using future-dated elections only when they become effective for the current pay period. If the election for a given plan type is equal to the current election, no entry is posted. If a participant is no longer eligible for a given plan type, that participant's current elections are terminated by the insertion of a row into the Base Benefit table for the plan type.
Inserting termination rows into the Base Benefit tables (rather than making a current row inactive) facilitates rolling back or reprocessing elections that have been posted to the Base Benefit tables. You can reverse Individual elections—or groups of participant elections—out of the Base Benefit tables by identifying those participants for reprocessing.
Note: If you were to look at the physical record structures underlying the Base Benefits election tables, you might notice that it still contains the fields Coverage End Date and Deduction End Date. This is for historical reasons only, and their use is discontinued, having been replaced by the approach of inserting superseding Termination, Waive, or Election rows. You should not create any processes that update these end date fields or any fields that rely on them.