Enrolling Participants in COBRA Coverage Manually
You can bypass the automated COBRA Administration batch process and force the system to enroll employees and dependents into COBRA health benefits.
When you bypass the batch process, participants do not require COBRA-qualifying events in order to be eligible for COBRA benefits. Instead, the system automatically gives all participants enrolled in COBRA coverage through these pages a COBRA event ID of 900.
Note: When you manually enroll an employee or dependent in COBRA coverage, subsequent COBRA processing, such as secondary event processing, is not aware of the manually enrolled COBRA coverage. When you add a nonemployee through COBRA, the nonemployee record may not show in other HR processes until the Refresh Personal Data process is run.
Warning! Because these pages ignore the processing rules that regulate COBRA coverage eligibility, manually process COBRA coverage only after careful consideration.
This section describes how to enroll participants in COBRA coverage manually.
|
Page Name |
Definition Name |
Usage |
|---|---|---|
|
CBR_MANUAL_ENT1 |
Manually establish an employee dependent as a nonemployee in preparation for manually enrolling the dependent into COBRA coverage. |
|
|
CBR_MANUAL_PARTIC1 |
Manually assign an employee or COBRA nonemployee to a benefit program or make changes to that manual assignment over time. |
|
|
CBR_MANUAL_HEALTH1 |
Enroll participants in COBRA health benefits manually. |
Use the Create COBRA Non-Employee page (CBR_MANUAL_ENT1) to manually establish an employee dependent as a nonemployee in preparation for manually enrolling the dependent into COBRA coverage.
Navigation:
This example illustrates the fields and controls on the Create COBRA Non-Employee page. You can find definitions for the fields and controls later on this page.
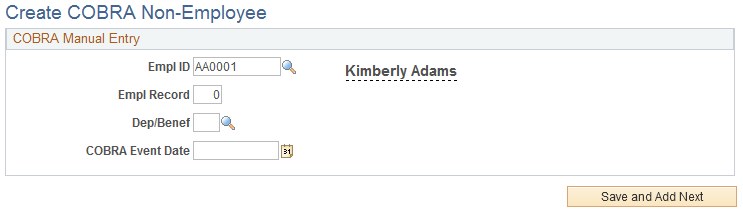
Field or Control |
Description |
|---|---|
Empl ID (employee ID) and Empl Record (employee record number) |
Enter the ID and employee record number for the employee whom the nonemployee participant is a dependent or beneficiary of. |
Dep/Benef (dependent/beneficiary) |
Enter the dependent or beneficiary number. |
COBRA Event Date |
Enter the event date for the nonemployee participant's COBRA enrollment. |
Save and Add Next |
Click to save the information. A message appears informing you of the COBRA employee ID assigned to this person. Note the new employee ID for the COBRA nonemployee and click OK. |
Use the Manual COBRA Benefit Program page (CBR_MANUAL_PARTIC1) to manually assign an employee or COBRA nonemployee to a benefit program or make changes to that manual assignment over time.
Navigation:
This example illustrates the fields and controls on the Manual COBRA Benefit Program page. You can find definitions for the fields and controls later on this page.
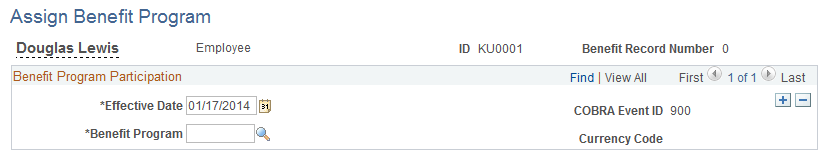
The benefit program is assigned a COBRA event ID of 900.
Use the Select Health Benefits page (CBR_MANUAL_HEALTH1) to enroll participants in COBRA health benefits manually.
Navigation:
This example illustrates the fields and controls on the Select Health Benefits page. You can find definitions for the fields and controls later on this page.
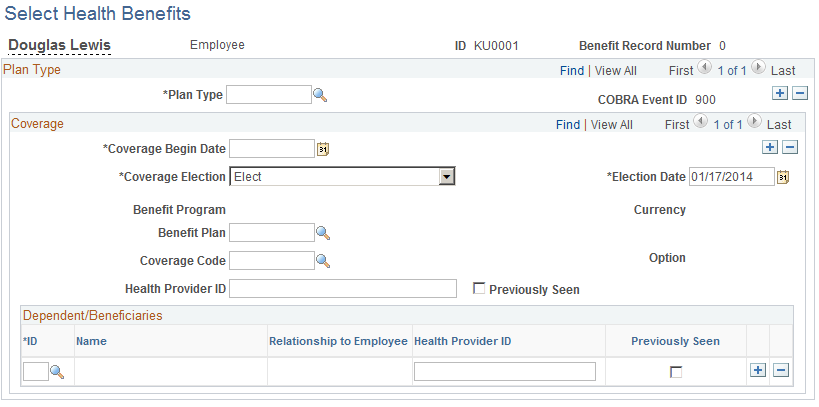
The health benefit record of the selected participant receives a COBRA event ID of 900.
Field or Control |
Description |
|---|---|
Coverage Begin Date |
Automatically set to the current date. |
Coverage Election |
Elect or terminate a benefit plan. |
Option |
The system displays the COBRA option that goes with the selected benefit plan. |
Health Provider ID |
Enter the name of the employee's doctor, an ID number, or any other format that the health provider may require. |
Previously Seen |
Select to indicate that the employee is a current patient of the indicated physician. Becomes available when you enter a health provider ID. |
HIPAA Report Date (Emp) |
Displays the date on which the employee's certificate of creditable health coverage was printed if health coverage was terminated. These certificates are guaranteed to employees by the Health Insurance and Accountability Act of 1996, and you can print them by running HIPAA reports. Note: The certificate of creditable coverage lists all group health coverage that an employee had for the 12–month period prior to the date that coverage ended. |
Dependent/Beneficiaries
Field or Control |
Description |
|---|---|
ID |
Select the dependent ID to add available beneficiaries to the selected COBRA participant/plan type/benefit plan combination. |
Relationship to Employee |
Identifies the dependent's relationship to the participant. |
Health Provider ID |
Enter the name of the employee's doctor, an ID number, or any other information that the health provider may require. |
Previously Seen |
Select to indicate that the employee is a current patient of the indicated physician. Becomes available when you enter a health provider ID. |