Specifying the Data to Extract
To define what data to extract, use the Enrollment Snapshot Options (BN_SNAP_CONFIG) component.
You can extract benefit plan types and other benefit-related information, such as deduction amounts, life and disability coverages, implied terminations, and the original enrollment date.
|
Page Name |
Definition Name |
Usage |
|---|---|---|
|
BN_SNAP_CONFIG |
Define data to extract from the database. |
Use the Enrollment Snapshot Options page (BN_SNAP_CONFIG) to define data to extract from the database.
Navigation:
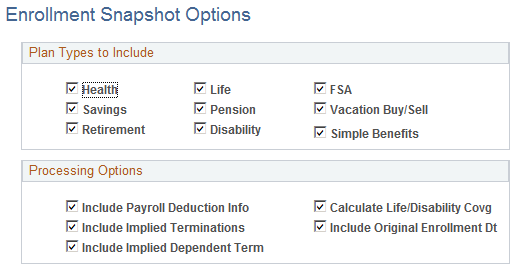
This example illustrates the fields and controls on the Enrollment Snapshot Options page. You can find definitions for the fields and controls later on this page.
Field or Control |
Description |
|---|---|
Plan Types to Include |
Select only the plan types for which you will create a carrier interface extract or transmit data to the Carrier Interface Supplier Integration process in eBenefits. Note: If you are running the snapshot process only to create a HIPAA EDI 834 file, check only the Health plan type to reduce the time necessary to populate the Snapshot tables. |
Include Payroll Deduction Info (include payroll deduction information) |
Select to include the last deduction taken and the pay end date for each enrollment. |
Calculate Life/Disability Covg (calculate life/disability coverage) |
Select to have the Enrollment Reporting Snapshot process calculate coverage for life and disability plans using the plan definitions, calculation rules, and employee's compensation rate or annual benefits base rate. |
Include Implied Term (include implied terminations) |
Select to include enrollments that are no longer valid because the participant has enrolled in another plan type, waived coverage, or transitioned to COBRA coverage. Note: You use this field whenever a carrier requires a positive notification of a termination or plan change (some carriers can detect these events simply by noticing a previous enrollment record). |
Include Implied Dependent Terminations |
Select to create termination records for dependents in the snapshot and report them in the HIPPA file when a termination of an employee also terminated the dependent or when new coverage has been added for an employee and a dependent who was previously covered has been dropped from coverage. Note: You must select Include Implied Employee Terminations, for Include Implied Dependent Termination to be functional. |
Include Original Enrollment Dt (include original enrollment date) |
Select to include an employee's earliest continuous enrollment date in the current, active plan. This applies only to employee-level enrollments and allocations. Changes to coverage codes in health plans, employee-specified coverage amounts in life and disability plans, or employee contribution amounts do not constitute a change in plan. This field applies to employees and dependents. |